When someone like Dr. Victor Han calls a technology a “game-changer” for children’s health care, you pay attention.
As Chair of the Division of Neonatal-Perinatal Medicine, Director of the Children’s Health Research Institute (CHRI) of the Lawson Health Research Institute and a Canada Research Chair in Maternal and Fetal Health, Dr. Han is a leading specialist in neonatal-perinatal medicine and paediatrics. If anyone knows about early childhood health, it’s Dr. Han.
Children’s Health Foundation donors have already made progress on funding Dr. Han’s game-changing technology, too.
The technology he’s working to bring to CHRI is called Olink. Dr. Han lights up with excitement when he speaks about it. As both a diagnostic and research tool, Olink holds remarkable promise that solves a few big issues with currently available technology.
When doctors want to find out what’s going on inside a patient, one of the first things they’ll do is draw blood. Many lessons can be learned by what’s in a patient’s blood, and especially in the plasma. The plasma is then subjected to a multitude of tests to determine what sorts of proteins are in there.
Your body is constantly shedding proteins that end up in your blood plasma. The proteins present, and the amounts they’re present in blood plasma, tell a story. Some proteins such as albumin, which is the most abundant protein in the plasma, will be produced in smaller amounts when a patient’s liver isn’t working well, for example.
The BIG Problem for Our Littlest Patients
The stories told by blood plasma can be critical to understanding a patient’s wellbeing, especially with patients who can’t tell doctors where the problems they’re experiencing are – for example, babies.
When a baby is born prematurely, weighing just a pound or less, their blood volume is incredibly low compared to an adult — preterm babies have about 50 mL of blood in their bodies, while an adult has about five to six litres of blood. So, for preterm babies, even a single drop of blood drawn to sample is a lot to lose. “If you take just 1 tsp or 5 mL of blood, the baby will go into shock,” Dr. Han explains. But the information contained in that sample can be critical to saving the infant’s life. To track a disease’s development, doctors will need to draw blood multiple times.
How Blood Plasma Is Currently Analyzed
Currently, blood plasma is analyzed through a couple of processes: mass spectrometry and immunoassays. As Dr. Han describes, in mass spectrometry, a sample is sprayed into the air while the machine emits light onto the sample. The light that reflects off the sample shows what proteins are present and in what concentrations. It’s a good technology, but it requires a significant sample size, and mass spectrometers tend to be large machines.
Immunoassays also represent good technology with limitations. It’s a test that uses your body’s immune system responders, antibodies, to react with the proteins in a blood sample. You’ve probably heard of an antigen test by now – it’s the same idea. Unfortunately, immunoassays occasionally come up with inaccurate results like false positives.
The Benefits of Olink Analysis
Where Olink differs is that the proteins are exposed to two antibodies developed specifically for each protein. The antibodies also have a strand of DNA attached to them that only a particular protein can possibly react with. There’s less chance of proteins and antibodies getting mixed up or confused.
The bottom line is that with Olink, a sample analysis will be faster, more accurate and specific while using a fraction of the sample volume needed compared to currently available technologies. Parents of a premature infant who can’t afford even a 5 mL blood draw need not worry — for an Olink analysis, all that’s needed is five microlitres. That’s 1,000 times less material.
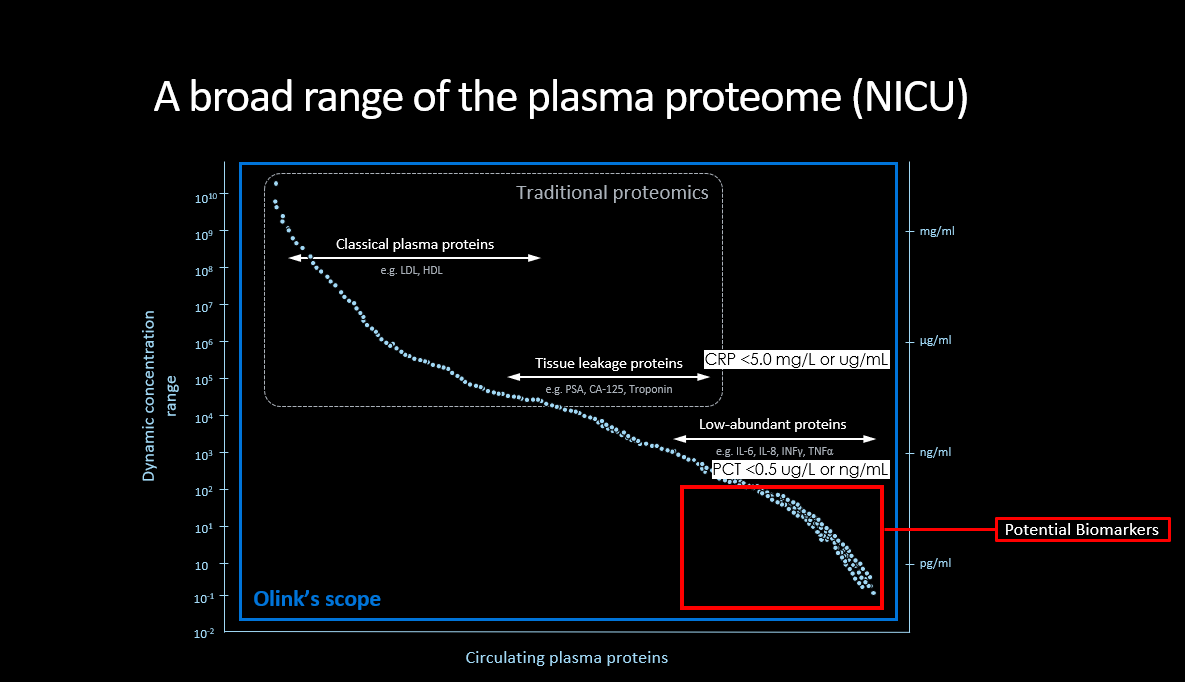
Olink’s ability to examine minuscule amounts allows researchers to delve to new depths. Most of the proteins in blood plasma exist at relatively large sizes and concentrations. However, some of the proteins that can inform clinicians about the state of their patients come in infinitesimally tiny amounts. We’re talking picograms, or a trillionth of a gram in less than a drop of blood.
The proteins present in blood plasma at that level fascinate researchers like Dr. Han. Those proteins exist in such minuscule quantities that researchers have difficulty identifying them with current technology. But there are thousands of them, and they’re not well understood. “People like myself have been trying to understand what these proteins are,” says Dr. Han.
Other Applications for Olink
Olink tests will be useful for those researching the known as well as the unknown. The sensitivity of Olink tests can pick up such small amounts of proteins that they can often detect signs of cancer before symptoms ever show up. That’s especially important for cancers like pancreatic cancer or ovarian cancer, which tend to progress to a dangerous point before they’re detected. Olink efficiently separates a needle in a haystack while virtually eliminating false positives.
It’s more than blood, too – Olink can test all kinds of fluids like urine, cerebrospinal fluid or saliva. In all, it can test for more than 5,000 proteins with incredible specificity.
Each blood sample is a snapshot that doctors and researchers can use to see a disease’s development. With Olink, doctors can take multiple snapshots over time increasing the understanding of how the disease is progressing, thus improving the accuracy with which doctors can predict the disease progress, and therefore, the patient’s future.
“As doctors, we want to be able to tell families and patients the prognosis,” says Dr. Han. “With Olink, we can now detect the specific cell types in a tissue, the damage and the extent of the damage the disease has inflicted, and can tell if this patient is going to turn out completely well, or if this patient is going to have some damage in this particular tissue and we need to look out for it, and then we can try to develop more treatments to minimize the damage.”
Simply put, Olink can find and read the proteins well enough for researchers to see what’s happening with a disease, predict what will happen, and help find new ways to fix the damage it causes.
Dr. Han and his colleague, Dr. Douglas Fraser, have already used Olink technology to examine covid patients and successfully predicted which patients will develop vascular issues, acute problems that need ICU care, long covid, or other issues.
As cutting-edge technology, CHRI’s Olink lab will be one of the first in Canada, right here in London. The time and cost savings from having to send samples as far away as Sweden or Boston for analysis are an attractive feature for clinicians in the area as well.
And for researchers like Dr. Han, Olink will allow them to study those thousands of tiny proteins and make new discoveries. They’ll be able to re-purpose drugs to counteract disease processes and develop precision therapies better able to target a particular disease.
As promising technologies go, Olink will indeed be a game-changer — and it will help shape the next 100 years of Children’s.