Establishing a New Standard of Care for Paediatric Epilepsy Patients
One of the gap areas identified within adolescent health are chronic conditions.
Epilepsy is a chronic condition in young people that impacts their mental health, relationship with food, sexual and reproductive health and requires transition to adult care.
The goal of robust holistic care of patients at Children’s Hospital, London Health Sciences Centre’s Paediatric Epilepsy Program is to be leaders in supporting patients and families in each of these priority areas impacted by epilepsy.
The program has a Comprehensive Epilepsy Clinic serving a large region of Western Ontario. As one of two Regional Centres of Excellence for Epilepsy Surgery in Ontario it now serves patients from across the province.

Children’s Hospital’s Paediatric Epilepsy Program is ready to expand its epilepsy treatment options for patients who have drug resistant epilepsy and aims to establish a new surgical standard of care that has proven successful with patients aged 10-18 years.
This type of surgery can cure seizures in these chronic patients with severe forms of drug resistant epilepsy. When seizures stop, the transformation can seem miraculous for both the patients and families and health outcomes can improve dramatically.
Children’s Hospital’s Paediatric Epilepsy Program has the exceptional leadership, multidisciplinary team and patient-family supports in place to expand its clinical capacity to use non-invasive robotic equipment for complex stereo electroencephalography (SEEG) procedures.
The group of candidates for SEEG procedures is growing and these children would have the chance to be cured of seizures and lead healthy lives. A transformational health outcome for young people that not only reduces restrictions, but also provides opportunities for healthy futures and quality of life improvements.
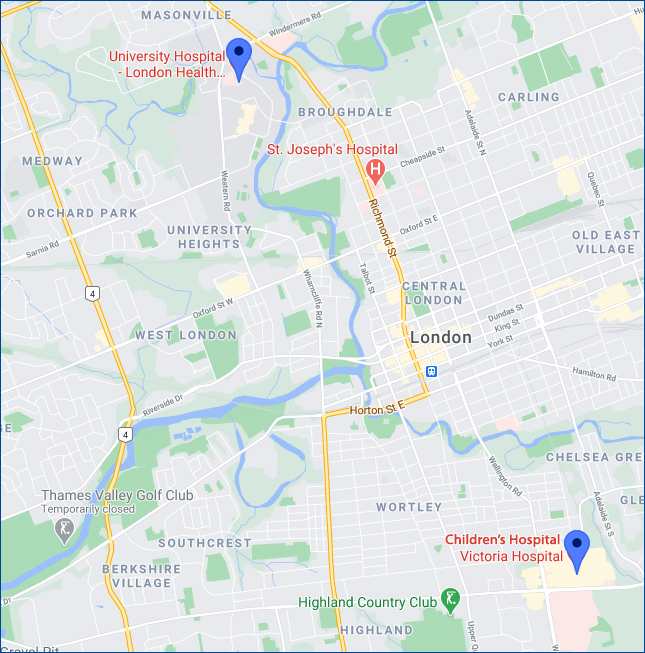
At the stage when families are ready to consider curative epilepsy surgery using SEEG procedures, the surgery cannot be carried out onsite at Children’s Hospital.
Patients and the whole clinical team must be transported across town on the day of the operation to a different campus in the adult epilepsy surgery division where only a few paediatric surgeries can be completed in a year.
The very first pediatric epilepsy patient in Ontario who underwent a robot-assisted brain surgery was operated on by The Paediatric Epilepsy Program at Children’s Hospital.
Ethan, 14, is a Children’s Hospital patient with drug resistant epilepsy.
His seizures escalated until he experienced three straight days of 15 to 20 second seizures, every couple of minutes.
Children's Hospital wants to help more patients like Ethan.
Meet ROSA
Having demonstrated the success of this surgery for patients with chronic epilepsy over the last two years, Children’s Hospital and its Paediatric Epilepsy Program is ready to expand with its own equipment and the necessary clinical program supports to make this treatment successful.
The ROSA SEEG Robotic arm serves the paediatric population.
Surgery using ROSA takes less time, is less invasive, more accurate and will allow the program to exponentially grow the number of patients whose lives can be dramatically improved. Expanding epilepsy treatment capacity would also mean Children’s Hospital’s Regional Centre of Excellence for Epilepsy Surgery in Ontario would be the first in the province to have this equipment which is now the standard of care in Europe and the United States.

Addressing 5 Pressing Priorities Within Adolescent Health:
Young people with epilepsy have a greater risk of mental illness than their healthy peers or even youth with other chronic disorders, such as diabetes.
Rates of anxiety and depression are particularly high among this population.
Additionally, suicide rates are five times higher than the average. Epilepsy patients struggle with the stigma associated with having seizures and experience fears about brain damage or death.
This project will support improved care for the most severely impacted epilepsy patients, to help them live life fully.
Patients who are part of the Comprehensive Epilepsy Clinic will have access to a clinical neuropsychologist who provides feedback to patients and their families, as well as to other members of the Epilepsy Team and consultation with schools may be provided.
In addition, patients have access to specialized mindfulness training designed for young epilepsy patients.
Young people with epilepsy have an increased risk of an eating disorder and poor‐quality diet.
Managing epilepsy also involves improving relationships with food. Children’s Hospital has increased the capability of the Ketogenic Dietary services with currently over 30 children who have been part of the program in the last two years.
The team will be creating educational videos for families to educate and explain the diet. Dr. Maryam Nouri and the dietician are also leading the Children’s, LHSC site for the EpLink provincial research collaboration in the ketogenic diet group.
Epilepsy may influence sexual function and behavior and medications can impact hormones.
Developmental delays, stigma and other factors play a part in developing healthy sexual and reproductive health. The social worker and epilepsy educator support young patients through these questions and families when seeking community support. Genetic testing and counselling are available through the epilepsy clinic.
The World Health Organization (WHO) defines epilepsy as, “a chronic noncommunicable disease of the brain. It is characterized by recurrent seizures. Seizures can vary from the briefest lapses of attention or muscle jerks to severe and prolonged convulsions. Seizures can also vary in frequency, from less than 1 per year to several per day.”
Epilepsy is one of the most common neurological conditions in the paediatric population, with an estimated 15,000 children in Ontario. Drug resistant epilepsy occurs when a child has failed at least two well‐chosen and well tolerated antiepileptic drugs and may require nonpharmacological therapies. Thirty percent of epilepsy patients have drug resistant epilepsy.
Young patients with epilepsy are more likely to have psychological problems, especially depression, anxiety and suicidal thoughts and behaviors. Problems may be a result of difficulties dealing with the condition itself as well as medication side effects.
At Children’s Hospital treating epilepsy has a range of approaches including psychosocial care.
The clinical services available to young patients and families at Children’s Hospital include: paediatric epilepsy monitoring unit; the comprehensive epilepsy clinic; genetic counselling; the shared decision making coach; the epilepsy surgery program; and the ketogenic diet and dietician. As well, the program is active with project ECHO, epilepsy across the life span.
Adolescence is a crucial time with many changes, including critical thinking, cognitive skills, and autonomy (individual choice), all of which make for a complicated jump to adult life.
An adolescent person with epilepsy may face additional challenges. The Transition Clinic is a process that prepares patients 16‐18 years old and their families for ‘adult’ health care and assists in navigating the adult health care world.
Children’s Hospital’s Peadiatric Epilepsy program uses an evidence‐based approach and has two types of transition clinics – one for patients who respond to medication and the second transition clinic is the Epilepsy Transition Clinic for youth who have been diagnosed with drug resistant epilepsy and are seen within the Comprehensive Epilepsy Clinic. They meet an Adult Epileptologist (Physician), Transition Specialist, and Paediatric Social Worker to discuss how treatment will look in the adult world and what extra supports are needed in the upcoming years to fully participate at home, in school and in the community.
To date, Children’s Health Foundation has supported several components of its exceptional epilepsy care from the development of the shared-decision making model to the Child Life Program, Family Assistance Program and including the evidence-based transition clinic.